Accuracy of Porto Alegre’s Line in predict lenticulostriate arteries encasement in insular gliomas
Marco Antônio Schlindwein Vaz1, Rafaela Fernandes Gonçalves1,2,3,4, Jander Moreira Monteiro1,2, Samir Aler Bark1,3, Viviane Buffon1, Samuel Dobrowolski1, Gustavo Rassier Isolan1,2,3,4
1 Centro Avançado de Neurologia e Neurocirurgia (CEANNE)
2 Spalt Therapeutics
3 Faculdade Evangélica Mackenzie do Paraná (FEMPAR)
4 National Science and Technology Institute for Children’s Cancer Biology and Pediatric Oncology – INCT BioOncoPed, Brazil (INCT)
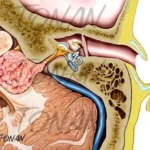
Purpose: The Insula is a common site of gliomas. Such lesions are of challenging surgical management because of complex anatomy of the lobe and the proximity to functional structures such as basal ganglia, internal capsule, speech and language processing cortex and subcortex as well as arteries like the middle cerebral artery and lenticulostriates arteries (LSTa). Brain mapping is quite challenging when the medial aspect of insular tumors does not displace but involve the LSTa. In these cases, even intensive efforts to preserve the integrity of the internal capsule based on subcortical mapping, results in no assurance that the patient will not experience a new motor or sensorial deficit in the postoperative period. This is the main reason why studying the relation of the LSA with the medial aspect of the insular tumors preoperatively and intraoperatively is of paramount importance.
Methods: A retrospective review of our database of 52 patients of insular glioma operated on by the senior author (GRI) between 2007 and 2018 was performed. For patients of insular gliomas undergoing awake surgery, our medial limit of resection, mainly in the tumor part located next to the limen of insula, was identified primarily through altered speech patterns, such as paraphasia during electric subcortical stimulation of the inferior fronto-occipital fasciculus (IFOF). To evaluate the potential involvement of LSA within the medial aspect of the tumor, we carried out an accurate analysis of the coronal and axial T2 and T1-weighted MR images and considered that the tumors that entangled these vessels could not be entirely resect.
Results: Lenticulostriate arteries involvement was determined from preoperative and intra-operative findings, as described above. In 13 patients LSTa were founded to be involved by the tumor. In 3 patients there were no involvement of the LSTa which has allowed a more aggressive resection. These findings may suggest that tumors with a medial putaminal invasion cannot be submitted to an almost complete resection without causing a serious neurological deficit. Most of these patients have a subtotal resection whatever approach is chosen (transsylvian or transcortical). Probably the LSTa involvement is the most important medial limiting factor to obtain a more aggressive tumor resection and a good overall survival as well (P=0.022).
Conclusion: We have found that LSTa encasement is limiting factor to reach a good EOR